Usuário:Vini 175/Doença de Behçet
Predefinição:Infobox disease
Behçet's disease or Behçet disease (/bɛˈtʃɛt/), sometimes called Behçet's syndrome, Morbus Behçet, Adamantiades syndrome, [1] or Silk Road disease, is a rare immune-mediated small-vessel systemic vasculitis[2] that often presents with mucous membrane ulceration and ocular problems. Behçet's disease (BD) was named in 1937 after the Turkish dermatologist Hulusi Behçet, who first described the triple-symptom complex of recurrent oral aphthous ulcers, genital ulcers, and uveitis. As a systemic disease, it can also involve visceral organs such as the gastrointestinal tract, pulmonary, musculoskeletal, cardiovascular and neurological systems. As the disease can affect nearly every organ in the body, other conditions such as vasculitis, fibromyalgia, migraines/central nervous system problems,[necessário esclarecer] eyesight problems, tachycardia and joint pain and swelling are also commonly linked to Behçet's Disease.{{carece de fontes}} This syndrome can be fatal due to ruptured vascular aneurysms or severe neurological complications.[3]
Causa[editar | editar código-fonte]
The cause is not well-defined, but it is primarily characterized by auto-inflammation of the blood vessels. Although sometimes erroneously referred to as a "diagnosis of exclusion," the diagnosis can sometimes be reached by pathologic examination of the affected areas.[4]
The primary mechanism of the damage is an overactive immune system that seems to target the patient's own body. The involvement of a subset of T cells (Th17) seems to be important.[5] The primary cause is not well known. In fact, no one knows yet why the immune system starts to behave this way in Behçet's disease. There does however seem to be a genetic component involved, as first degree relatives of the affected patients are often affected in more than expected proportion for the general population. {{carece de fontes}}
An association with the GIMAP family of genes on the long arm of chromosome 7 (7q36.1) has been reported.[6] The genes implicated were GIMAP1, GIMAP2 and GIMAP4.
Fisiopatologia[editar | editar código-fonte]

Behçet's disease is considered more prevalent in the areas surrounding the old silk trading routes in the Middle East and in Central Asia. Thus, it is sometimes known as Silk Road Disease. However, this disease is not restricted to people from these regions. A large number of serological studies show a linkage between the disease and HLA-B51.[8] HLA-B51 is more frequently found from the Middle East to South Eastern Siberia, but the incidence of B51 in some studies was 3 fold higher than the normal population. However, B51 tends not to be found in disease when a certain SUMO4 gene variant is involved,[9] and symptoms appear to be milder when HLA-B27 is present.[10] At the current time, a similar infectious origin has not yet been confirmed that leads to Behçet's disease, but certain strains of Streptococcus sanguinis has been found to have a homologous antigenicity.[11]
Vasculitis resulting in occlusion of the vessels supplying the optic nerve may be the cause of acute optic neuropathy and progressive optic atrophy in Behçet's disease. Histological evaluation in a reported case of acute optic neuropathy demonstrated substitution of the axonal portion of the optic nerve with fibrous astrocytes without retinal changes.[12] CNS involvement in Behçet's may lead to intracranial hypertension most commonly due to dural venous sinus thrombosis[13] [8-10] and subsequent secondary optic atrophy.
Sinais e sintomas[editar | editar código-fonte]

Pele e mucosas[editar | editar código-fonte]
Quase todos os pacientes se apresentam com ulcerações orais mucocutâneas dolorosas na forma de aftas ou ulcerações mucocutâneas não cicatrizantes.[3] As lesões orais são similares àquelas encontradas na doença inflamatória intestinal e podem reincidir.[3] Úlceras genitais dolorosas geralmente se desenvolvem ao redor do ânus, da vulva ou do escroto, repetindo-se em 75% dos pacientes.[3] Além disso, os pacientes podem se apresentar com eritema nodoso, vasculite pustular cutânea e lesões similares ao pioderma gangrenoso.[3]
Sistema ocular[editar | editar código-fonte]
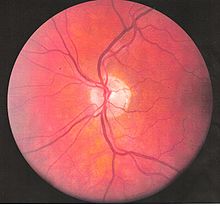
Pode haver desenvolvimento de doença inflamatória ocular já nos estágios iniciais da doença, levando a uma perda permanente da visão em 20% dos casos. O envolvimento ocular pode se dar na forma de uveíte posterior, uveíte anterior ou vasculite retiniana. A uveíte anterior se apresenta com dor nos olhos, derrame conjuntival, hipópio e redução da acuidade visual, enquanto na uveíte posterior não há dor, mas cursa com redução da acuidade visual e alterações do campo visual. Uma forma rara de envolvimento ocular nesta síndrome é a vasculite retininana, que se apresenta com redução não dolorosa da visão com a possibilidade de alterações do campo visual.
O acometimento do nervo óptico na doença de Behçet é raro, se apresentando tipicamente como atrofia óptica progressiva e perda visual. Entretanto, casos de neuropatia óptica aguda (especificamente neuropatia óptica isquêmica anterior) já foram relatados.[14] A atrofia do nervo óptico tem sido identificada como a causa mais comum de dano à visão. A doença de Behçet pode resultar em envolvimento primário ou secundário do nervo óptico. Papiledema, como resultado de trombose de seio dural,[13] e atrofia resultante de doença retiniana têm sido caracterizados como causas secundárias de atrofia do nervo óptico na doença de Behçet.[15][12]
Sinais e sintomas de neuropatia óptica aguda incluem perda visual indolor, que pode afetar somente um dos olhos ou os dois, redução da visão de cores, defeito pupilar aferente relativo, escotoma central, edema do disco óptico, edema macular ou dor retrobulbar. Quando esses sintomas ocorrem simultâneos a ulcerações mucocutâneas, levantam a suspeita de neuropatia óptica aguda na doença de Behçet. A atrofia óptica progressiva pode resultar em redução da acuidade visual ou da visão de cores. Hipertensão intracraniana com papiledema pode estar presente.
Sistema gastrointestinal[editar | editar código-fonte]
As manifestações gastrointestinais incluem dor abdominal, náuseas e diarreia, que pode ser sanguinolenta. Frequentemente, há envolvimento da válvula ileocecal.[3] Muitos pacientes com doença de Behçet reclamam de sensibilidade abdominal, inchaço e desconforto abdominal geral, que pode imitar uma síndrome do intestino irritável.
Sistema respiratório[editar | editar código-fonte]
O acometimento pulmonar ocorre tipicamente na forma de hemoptise, pleurite, tosse ou febre. Em casos mais graves, pode haver risco de morte se houver desenvolvimento de aneurisma da artéria pulmonar seguida de ruptura, causando grave colapso vascular e morte por hemorragia nos pulmões.[3] Nódulos, consolidações, cavidades e lesões em vidro fosco são comuns em pacientes com envolvimento pulmonar.[5] Pode ocorrer trombose da artéria pulmonar.
Sistema musculoesquelético[editar | editar código-fonte]
Artralgia é observada em mais da metade dos pacientes e, em geral, trata-se de poli ou oligoartrite não erosiva principalmente nas grandes articulações dos membros inferiores.[3]
Sistema nervoso[editar | editar código-fonte]
O envolvimento do sistema nervoso central é mais frequente na forma de uma meningoencefalite crônica. As lesões tendem a ocorrer no tronco encefálico, nos gânglios basais e na substância branca profunda dos hemisférios e podem se assemelhar com as lesões da esclerose múltipla. A atrofia do tronco encefálio é observada em casos crônicos.
O acomentimento neurológico varia de uma meningite asséptica a uma trombose vascular, como a trombose de seio dural, manifestando-se com confusão, convulsões e perda de memória.[3] Frequentemente, surge mais tarde no progresso da doença, mas está associado a um mau prognóstico.
Sistema cardiovascular[editar | editar código-fonte]
A pericardite é uma manifestação cardíaca frequente.[5] A regurgitação aórtica crônica devido a doença da raiz aórtica também pode ser observada.[16]
Diagnóstico[editar | editar código-fonte]
There is no specific pathological testing or technique available for the diagnosis of the disease, although the International Study Group criteria for the disease are highly sensitive and specific, involving clinical criteria and a pathergy test.[3][17] Behçet's disease has a high degree of resemblance to diseases that cause mucocutaneous lesions such as Herpes simplex labialis, and therefore clinical suspicion should be maintained until all the common causes of oral lesions are ruled out from the differential diagnosis.
Visual acuity, or color vision loss with concurrent mucocutaneous lesions and/or systemic Behçet's symptoms should raise suspicion of optic nerve involvement in Behçet's disease and prompt a work-up for Behçet's disease if not previously diagnosed in addition to an ocular work-up. Diagnosis of Behçet's disease is based on clinical findings including oral and genital ulcers, skin lesions such as erythema nodosum, acne, or folliculitis, ocular inflammatory findings and a pathergy reaction. Inflammatory markers such ESR, and CRP may be elevated. A complete ophthalmic examination may include a slit lamp examination, optical coherence tomography to detect nerve loss, visual field examinations, fundoscopic examination to assess optic disc atrophy and retinal disease, fundoscopic angiography, and visual evoked potentials, which may demonstrate increased latency. Optic nerve enhancement may be identified on Magnetic Resonance Imaging (MRI) in some patients with acute optic neuropathy. However, a normal study does not rule out optic neuropathy. Cerebrospinal fluid (CSF) analysis may demonstrate elevated protein level with or without pleocytosis. Imaging including angiography may be indicated to identify dural venous sinus thrombosis as a cause of intracranial hypertension and optic atrophy.
Critérios diagnósticos[editar | editar código-fonte]

According to the International Study Group guidelines, for a patient to be diagnosed with Behçet's disease,[17] the patient must have oral (aphthous) ulcers (any shape, size, or number at least 3 times in any 12 months period) along with 2 out of the following 4 "hallmark" symptoms:
- genital ulcers (including anal ulcers and spots in the genital region and swollen testicles or epididymitis in men)
- skin lesions (papulo-pustules, folliculitis, erythema nodosum, acne in post-adolescents not on corticosteroids)
- eye inflammation (iritis, uveitis, retinal vasculitis, cells in the vitreous)
- pathergy reaction (papule >2 mm dia. 24-48 hrs or more after needle-prick). The pathergy test has a specificity of 95% to 100%, but the results are often negative in American and European patients[3]
Despite the inclusive criteria set forth by the International Study Group, there are cases where not all the criteria can be met and therefore a diagnosis cannot readily be made. There is however a set of clinical findings that a physician can rely upon in making a tentative diagnosis of the disease; essentially Behçet's disease does not always follow the International Study Group guidelines and so a high degree of suspicion for a patient who presents having any number of the following findings is necessary:
- mouth ulcers
- arthritis/arthralgia
- nervous system symptoms
- stomach and/or bowel inflammation
- deep vein thrombosis
- superficial thrombophlebitis
- epididymitis
- cardio-vascular problems of an inflammatory origin
- inflammatory problems in chest and lungs
- problems with hearing and/or balance
- extreme exhaustion
- changes of personality, psychoses
- any other members of the family with a diagnosis of Behçet disease.
Tratamento[editar | editar código-fonte]
Current treatment is aimed at easing the symptoms, reducing inflammation, and controlling the immune system. High dose Corticosteroid therapy (1 mg/kg/d oral prednisone) is indicated for severe disease manifestations.[18] Anti-TNF therapy such as infliximab has shown promise in treating the uveitis associated with the disease.[19][20] Another Anti-TNF agent, Etanercept, may be useful in patients with mainly skin and mucosal symptoms.[21]
Interferon alfa-2a may also be an effective alternative treatment, particularly for the genital and oral ulcers[22] as well as ocular lesions.[23] Azathioprine, when used in combination with interferon alfa-2b also shows promise,[24] and Colchicine can be useful for treating some genital ulcers, erythema nodosum, and arthritis.[25]
Thalidomide has also been used due to its immune-modifying effect.[26] Dapsone and rebamipide have been shown, in small studies, to have beneficial results for mucocutaneous lesions.[27][28]
Given its rarity, the optimal treatment for acute optic neuropathy in Behçet's disease has not been established. Early identification and treatment is essential. Response to ciclosporin, periocular triamcinolone, and IV methylprednisone followed by oral prednisone has been reported although relapses leading to irreversible visual loss may occur even with treatment.[29] Immunosuppressants such as interferon alpha and tumour necrosis factor antagonists may improve though not completely reverse symptoms of ocular Behçet's, which may progress over time despite treatment. When symptoms are limited to the anterior chamber of the eye prognosis is improved. Posterior involvement, particularly optic nerve involvement is a poor prognostic indicator. Secondary optic nerve atrophy is frequently irreversible. Lumbar puncture or surgical treatment may be required to prevent optic atrophy in cases of intracranial hypertension refractory to treatment with immunomodulators and steroids.
IVIG could be a treatment for severe[30] or complicated cases.[31][32]
Epidemiologia[editar | editar código-fonte]
The syndrome is rare in the United States, but is common in the Middle East and Asia, suggesting a possible cause endemic to the tropical areas.[33] It is not associated with cancer, and links with tissue-types (which are under investigation) are not certain. It also does not follow the usual pattern for autoimmune diseases. However, one study has revealed a possible connection to food allergies, particularly to dairy products.[34] An estimated 15,000 to 20,000 Americans have been diagnosed with this disease. In the UK, it is estimated to have about 1 case for every 100,000 people.[35] Globally, males are affected more frequently than females.[36] In the United States, more females are affected than males.{{carece de fontes}}
In an epidemiologic study, 56% of patients with Behçet's disease developed ocular involvement at a mean age of 30.[37] Ocular involvement was the first manifestation of Behçet's disease in 8.6% of patients.[37] Ocular Behçet's with involvement of the optic nerve is rarely reported. Among patients with ocular Behçet's disease funduscopic findings of optic atrophy, and optic disc paleness have been identified with a frequency of 17.9% and 7.4%, respectively. Other fundoscopic findings include vascular sheathing (23.7%),[15] retinal hemorrhage(9%),[15] macular edema(11.3%),[15] branch retinal vein occlusion(5.8%),[15] and retinal edema (6.6%).[15] However, optic atrophy was the most significant cause of visual impairment identified in 54% of patients with ocular Behçet's disease and permanent visual impairment.[15]
The prevalence of this disease increases from North to South. It follows a more severe course in patients with an early age of onset particularly in patients with eye and gastrointestinal involvement.[38]
Na gravidez[editar | editar código-fonte]
With Behçet's as an intercurrent disease in pregnancy, the pregnancy does not have an adverse effect on the course of Behçet's disease and may possibly ameliorate its course.[39][40] Still, there is a substantial variability in clinical course between patients and even for different pregnancies in the same patient.[39] Also, the other way around, Behçet's disease confers an increased risk of pregnancy complications, miscarriage and Cesarean section.[40]
História[editar | editar código-fonte]
Behçet disease is named after Hulusi Behçet (1889–1948), the Turkish dermatologist and scientist who first recognized the syndrome in one of his patients in 1924 and reported his research on the disease in Journal of Skin and Venereal Diseases in 1936.[41][42] The name (Morbus Behçet) was formally adopted at the International Congress of Dermatology in Geneva in September 1947. Symptoms of this disease may have been described by Hippocrates in the 5th century BC, in his Epidemion (book 3, case 7).[43] Its first modern formal description was published in 1922.[41]
Some sources use the term "Adamantiades' syndrome" or "Adamandiades-Behçet syndrome", for the work done by Benediktos Adamantiades.[44] However, the current World Health Organization/ICD-10 standard is "Behçet's disease". In 1991, Saudi Arabian medical researchers described neuro-Behçet's disease,[45] a neurological involvement in Behçet's disease, considered one of the most devastating manifestations of the disease.[46] The mechanism can be immune-mediated or thrombotic.[47] The term dates back to at least 1990.[48]
Referências[editar | editar código-fonte]
- ↑ Neville BW, Damm DD, Allen CM, Bouquot JE. (2008). Oral & maxillofacial pathology 3rd ed. Philadelphia: W.B. Saunders. p. 336. ISBN 978-1416034353
- ↑ «Glossary,». Consultado em 28 de março de 2009. Cópia arquivada em 19 April 2009 Verifique data em:
|arquivodata=(ajuda) - ↑ a b c d e f g h i j k Bolster MB (2009). MKSAP 15 Medical Knowledge Self-assessment Program: Rheumatology. Philadelphia, Pa: American College of Physicians. ISBN 1-934465-30-5
- ↑ «Behcet Disease: Overview - eMedicine Dermatology». Consultado em 28 de março de 2009
- ↑ a b c Hatemi G, Seyahi E, Fresko I, Hamuryudan V (2012) Behçet's syndrome: a critical digest of the recent literature. Clin Exp Rheumatol
- ↑ Lee, YJ; Horie, Y; Wallace, GR; Choi, YS; Park, JA; Choi, JY; Song, R; Kang, YM; Kang, SW; Baek, HJ; Kitaichi, N; Meguro, A; Mizuki, N; Namba, K; Ishida, S; Kim, J; Niemczyk, E; Lee, EY; Song, YW; Ohno, S; Lee, EB (Sep 1, 2013). «Genome-wide association study identifies GIMAP as a novel susceptibility locus for Behcet's disease.». Annals of the rheumatic diseases. 72 (9): 1510–6. PMID 23041938. doi:10.1136/annrheumdis-2011-200288 Verifique data em:
|data=(ajuda) - ↑ Ohno S, Ohguchi M, Hirose S, Matsuda H, Wakisaka A, Aizawa M (September 1982). «Close association of HLA-Bw51 with Behçet's disease». Arch. Ophthalmol. 100 (9): 1455–8. PMID 6956266. doi:10.1001/archopht.1982.01030040433013 Verifique data em:
|data=(ajuda) - ↑ Durrani K, Papaliodis GN (2008). «The genetics of Adamantiades-Behcet's disease». Semin Ophthalmol. 23 (1): 73–9. PMID 18214795. doi:10.1080/08820530701745264
- ↑ Hou S, Yang P, Du L, Zhou H, Lin X, Liu X, Kijlstra A (October 2008). «SUMO4 gene polymorphisms in Chinese Han patients with Behcet's disease». Clin. Immunol. 129 (1): 170–5. PMID 18657476. doi:10.1016/j.clim.2008.06.006 Verifique data em:
|data=(ajuda) - ↑ Ahn JK, Park YG (October 2007). «Human leukocyte antigen B27 and B51 double-positive Behçet uveitis». Arch. Ophthalmol. 125 (10): 1375–80. PMID 17923546. doi:10.1001/archopht.125.10.1375 Verifique data em:
|data=(ajuda) - ↑ Yanagihori H, Oyama N, Nakamura K, Mizuki N, Oguma K, Kaneko F (July 2006). «Role of IL-12B promoter polymorphism in Adamantiades-Behcet's disease susceptibility: An involvement of Th1 immunoreactivity against Streptococcus Sanguinis antigen». J. Invest. Dermatol. 126 (7): 1534–40. PMID 16514412. doi:10.1038/sj.jid.5700203 Verifique data em:
|data=(ajuda) - ↑ a b Kansu T, Kirkali P, Kansu E, Zileli T (December 1989). «Optic neuropathy in Behçet's disease». J Clin Neuroophthalmol. 9 (4): 277–80. PMID 2531168 Verifique data em:
|data=(ajuda) - ↑ a b Fujikado, T; Imagawa K (1994). «Dural sinus thrombosis in Behçet's disease—a case report». Japanese Journal of Ophthalmology. 38 (4): 411–416. PMID 7723211
- ↑ Eye (7 de janeiro de 2011). «Access : A case of anterior ischemic optic neuropathy associated with Behcet's disease : Eye». Nature.com. Consultado em 3 de agosto de 2011
- ↑ a b c d e f g Ozdal PC, Ortaç S, Taşkintuna I, Firat E (2002). «Posterior segment involvement in ocular Behçet's disease». Eur J Ophthalmol. 12 (5): 424–31. PMID 12474927
- ↑ editors, Steven S. Agabegi, Elizabeth Agabegi ; contributing author, Adam C. Ring. Step-up to medicine 3rd ed. ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins. p. 266. ISBN 978-1609133603
- ↑ a b International Study Group for Behçet's Disease (May 1990). «Criteria for diagnosis of Behçet's disease». Lancet. 335 (8697): 1078–80. PMID 1970380. doi:10.1016/0140-6736(90)92643-V Verifique data em:
|data=(ajuda) Erro de citação: Código<ref>inválido; o nome "pmid1970380" é definido mais de uma vez com conteúdos diferentes - ↑ CMDT (Current Medical Diagnosis & Treatment) 2007, Chapter 20, page 872
- ↑ Sfikakis PP, Theodossiadis PG, Katsiari CG, Kaklamanis P, Markomichelakis NN (2001). «Effect of infliximab on sight-threatening panuveitis in Behcet's disease». Lancet. 358 (9278): 295–6. PMID 11498218. doi:10.1016/S0140-6736(01)05497-6
- ↑ Sfikakis PP (2002). «Behçet's disease: a new target for anti-tumour necrosis factor treatment». Ann Rheum Dis. 61 Suppl 2 (Suppl 2): ii51–3. PMC 1766720
 . PMID 12379622. doi:10.1136/ard.61.suppl_2.ii51
. PMID 12379622. doi:10.1136/ard.61.suppl_2.ii51
- ↑ Melikoglu M, Fresko I, Mat C, Ozyazgan Y, Gogus F, Yurdakul S, Hamuryudan V, Yazici H (2005). «Short-term trial of etanercept in Behcet's disease: a double blind, placebo controlled study». J Rheumatol. 32 (1): 98–105. PMID 15630733
- ↑ Alpsoy E, Durusoy C, Yilmaz E, Ozgurel Y, Ermis O, Yazar S, Basaran E (2002). «Interferon alfa-2a in the treatment of Behcet disease: a randomized placebo-controlled and double-blind study». Arch Dermatol. 138 (4): 467–71. PMID 11939808. doi:10.1001/archderm.138.4.467
- ↑ Kotter I, Zierhut M, Eckstein AK, Vonthein R, Ness T, Gunaydin I, Grimbacher B, Blaschke S, Meyer-Riemann W, Peter HH, Stubiger N (2003). «Human recombinant interferon alfa-2a for the treatment of Behçet's disease with sight threatening posterior or panuveitis». Br J Ophthalmol. 87 (4): 423–31. PMC 1771623
 . PMID 12642304. doi:10.1136/bjo.87.4.423
. PMID 12642304. doi:10.1136/bjo.87.4.423
- ↑ Hamuryudan V, Ozyazgan Y, Fresko Y, Mat C, Yurdakul S, Yazici H (2002). «Interferon alfa combined with azathioprine for the uveitis of Behcet's disease: an open study». Isr Med Assoc J. 4 (11 Suppl): 928–30. PMID 12455182
- ↑ Yurdakul S, Mat C, Tuzun Y, Ozyazgan Y, Hamuryudan V, Uysal O, Senocak M, Yazici H (2001). «A double-blind trial of colchicine in Behcet's syndrome». Arthritis Rheum. 44 (11): 2686–92. PMID 11710724. doi:10.1002/1529-0131(200111)44:11<2686::AID-ART448>3.0.CO;2-H
- ↑ Hamuryudan V, Mat C, Saip S, Ozyazgan Y, Siva A, Yurdakul S, Zwingenberger K, Yazici H (1998). «Thalidomide in the treatment of the mucocutaneous lesions of the Behcet syndrome. A randomized, double-blind, placebo-controlled trial». Ann Intern Med. 128 (6): 443–50. PMID 9499327. doi:10.7326/0003-4819-128-6-199803150-00004
- ↑ Matsuda T, Ohno S, Hirohata S, Miyanaga Y, Ujihara H, Inaba G, Nakamura S, Tanaka S, Kogure M, Mizushima Y (2003). «Efficacy of rebamipide as adjunctive therapy in the treatment of recurrent oral aphthous ulcers in patients with Behcet's disease: a randomised, double-blind, placebo-controlled study». Drugs R D. 4 (1): 19–28. PMID 12568631. doi:10.2165/00126839-200304010-00002
- ↑ Sharquie KE, Najim RA, Abu-Raghif AR (2002). «Dapsone in Behcet's disease: a double-blind, placebo-controlled, cross-over study». J Dermatol. 29 (5): 267–79. PMID 12081158
- ↑ Voros GM, Sandhu SS, Pandit R (2006). «Acute optic neuropathy in patients with Behçet's disease. Report of two cases». Ophthalmologica. 220 (6): 400–5. PMID 17095888. doi:10.1159/000095869
- ↑ Seider N, Beiran I, Scharf J, Miller B (November 2001). «Intravenous immunoglobulin therapy for resistant ocular Behçet's disease». Br J Ophthalmol. 85 (11): 1287–8. PMC 1723778
 . PMID 11673289. doi:10.1136/bjo.85.11.1287 Verifique data em:
. PMID 11673289. doi:10.1136/bjo.85.11.1287 Verifique data em: |data=(ajuda) - ↑ Shutty B, Garg KJ, Swender D, Chernin L, Tcheurekdjian H, Hostoffer R (July 2012). «Optimal use of ivig in a patient with Behçet syndrome and common variable immunodeficiency». Ann. Allergy Asthma Immunol. 109 (1): 84. PMID 22727170. doi:10.1016/j.anai.2012.05.014 Verifique data em:
|data=(ajuda) - ↑ Beales IL (December 1998). «Gastrointestinal involvement in Behçet's syndrome». Am. J. Gastroenterol. 93 (12): 2633. PMID 9860455. doi:10.1111/j.1572-0241.1998.02633.x Verifique data em:
|data=(ajuda) - ↑ Behcet's syndrome (Medline Plus).
- ↑ Triolo G, Accardo-Palumbo A, Dieli F, Ciccia F, Ferrante A, Giardina E, Licata G (May 2002). «Humoral and cell mediated immune response to cow's milk proteins in Behçet's disease». Ann. Rheum. Dis. 61 (5): 459–62. PMC 1754076
 . PMID 11959773. doi:10.1136/ard.61.5.459 Verifique data em:
. PMID 11959773. doi:10.1136/ard.61.5.459 Verifique data em: |data=(ajuda) - ↑ Behcet's disease.
- ↑ Escudier M, Bagan J, Scully C (March 2006). «Number VII Behçet's disease (Adamantiades syndrome)». Oral Dis. 12 (2): 78–84. PMID 16476027. doi:10.1111/j.1601-0825.2005.01144.x Verifique data em:
|data=(ajuda) - ↑ a b Krause L, Köhler AK, Altenburg A, Papoutsis N, Zouboulis CC, Pleyer U, Stroux A, Foerster MH (May 2009). «Ocular involvement in Adamantiades-Behçet's disease in Berlin, Germany». Graefes Arch. Clin. Exp. Ophthalmol. 247 (5): 661–6. PMID 18982344. doi:10.1007/s00417-008-0983-4 Verifique data em:
|data=(ajuda) - ↑ Hatemi G, Seyahi E, Fresko I, Hamuryudan V (2013) Behçet's syndrome: a critical digest of the 2012-2013 literature. Clin Exp Rheumatol 31(3 Suppl 77):108-117
- ↑ a b PMID 12928538 (PubMed)
- ↑ a b PMID 16167908 (PubMed)
- ↑ a b synd/1863 (em inglês) no Who Named It?
- ↑ H. Behçet. Über rezidivierende, aphtöse, durch ein Virus verursachte Geschwüre am Mund, am Auge und an den Genitalien. Dermatologische Wochenschrift, Hamburg, 1937, 105(36): 1152-1163. Reproduced in Viggor SF, Willis AM, Jawad ASM (2011). «Behçet's disease». Grand Rounds. 11: L1–L2. doi:10.1102/1470-5206.2011.L001
- ↑ Verity D H, Wallace G R, Vaughan R W, Stanford M R (29 de abril de 2003). «Behçet's disease: from Hippocrates to the third millennium». Ncbi.nlm.nih.gov. Consultado em 9 de janeiro de 2014
- ↑ B. Adamandiades. Sur un cas d'iritis à hypopyon récidivant. Annales d'oculistique, Paris, 1931, 168: 271-278.
- ↑ Malhotra Ravi (2004). «Saudi Arabia». Practical Neurology. 4 (3): 184–185. doi:10.1111/j.1474-7766.2004.03-225.x
- ↑ S. Saleem (2005), Neuro-Behçet's Disease: NBD, Neurographics, Vol. 4, Issue 2, Article 1.
- ↑ Al-Araji A, Kidd DP (February 2009). «Neuro-Behçet's disease: epidemiology, clinical characteristics, and management». Lancet Neurol. 8 (2): 192–204. PMID 19161910. doi:10.1016/S1474-4422(09)70015-8 Verifique data em:
|data=(ajuda) - ↑ Su SL, Way LJ, Lin RT, Peng MJ, Wu SC (March 1990). «Neuro-Behçet's disease: report of three cases with a review of the literature». Gaoxiong Yi Xue Ke Xue Za Zhi. 6 (3): 155–62. PMID 2188002 Verifique data em:
|data=(ajuda)
Leitura adicional[editar | editar código-fonte]
- Yamauchi Y, Cruz JM, Kaplan HJ, Goto H, Sakai J, Usui M (2005). «Suspected simultaneous bilateral anterior ischemic optic neuropathy in a patient with Behçet's disease». Ocul. Immunol. Inflamm. 13 (4): 317–25. PMID 16159724. doi:10.1080/09273940590950945
- Brissaud P, Laroche L, de Gramont A, Krulik M (March 1985). «Digital angiography for the diagnosis of dural sinus thrombosis in Behçet's disease». Arthritis Rheum. 28 (3): 359–60. PMID 3884020. doi:10.1002/art.1780280323 Verifique data em:
|data=(ajuda) - el-Ramahi KM, al-Kawi MZ (September 1991). «Papilloedema in Behçet's disease: value of MRI in diagnosis of dural sinus thrombosis». J. Neurol. Neurosurg. Psychiatr. 54 (9): 826–9. PMC 1014525
 . PMID 1955903. doi:10.1136/jnnp.54.9.826 Verifique data em:
. PMID 1955903. doi:10.1136/jnnp.54.9.826 Verifique data em: |data=(ajuda) - Fujikado T, Imagawa K (1994). «Dural sinus thrombosis in Behçet's disease—a case report». Jpn. J. Ophthalmol. 38 (4): 411–6. PMID 7723211
Ligações externas[editar | editar código-fonte]
Predefinição:Systemic connective tissue disorders Predefinição:Oral pathology

